What is Frozen Shoulder?
Adhesive capsulitis, also known as frozen shoulder, is a gradual loss of movement in the
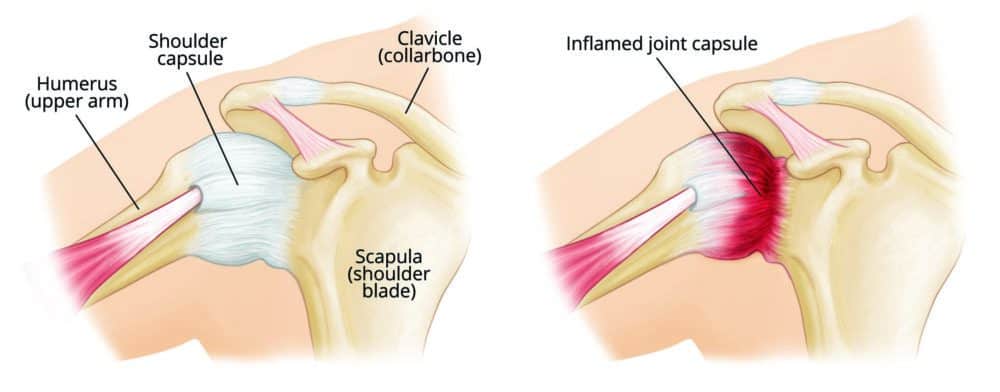
shoulder joint with associated pain. For starters, let’s go over a little bit of shoulder anatomy. The shoulder joint being the most mobile joint in the body consists of a ball and socket – the ball being the arm bone (humerus) and the socket being the shoulder blade (scapula). The humerus fits into the relatively shallow socket of the scapula in which is stabilized by our shoulder capsule which surrounds the entire joint. For ease of shoulder movement, we have synovial fluid that lubricates the shoulder capsule – this allows us to effortless carry out our day-to-day tasks with our arms. In frozen shoulder, the shoulder capsule becomes inflamed and over time thickens making the shoulder feel stiff and tight.
What are the symptoms of Frozen Shoulder?
- Pain of gradual onset and increasing severity (described often as a dull aching)
- Disturbed sleep
- Early stages are associated with pain at rest and with motion
- Gradual restriction in range of motion
- Difficulties with activities involving reaching overhead or behind back (i.e. brushing hair)
What are the causes of Frozen Shoulder?
The cause of frozen shoulder is not fully understood. With that being said, it typically occurs in one of two ways.
1) Insidiously – in other words, occurs for unknown reason or as a progression of another
injury. One theory is due to changing hormone levels as we age, which can affect both males and females. However, frozen shoulder is more commonly seen in women than in men. Another correlation found with frozen shoulder is the association with specific diseases. Some of these diseases include:
- Diabetes
- Hypothyroidism
- Hyperthyroidism
- Cardiovascular diseases
2) Resulting from another injury – a common cause of frozen shoulder is the immobility
after a shoulder injury. For example, when we injure a body part, we will tend to not move it as much to prevent pain. For the shoulder specifically, this injury can be a rotator cuff injury, a broken/fractured humerus, a stroke or post-surgical. After suffering one of
these injuries, prolonged immobilization can increase the risk of frozen shoulder.

What are the stages of Frozen Shoulder?
Stage 1: Freezing
In this early stage, there is typically sharp pain with movements, achy pain at rest, as well as sleep disturbances. The range of motion of the shoulder will also begin to be affected.
Stage 2: Frozen
In this stage, the pain may improve in the shoulder, however there is significant range of motion restrictions. Daily activities such as cleaning, getting dressed, and lifting will be greatly affected.
Stage 3: Thawing
In this stage, the pain is continuing to improve. The shoulder range of motion will slowly begin to be improved. Normal activities will also begin to feel normal again.
This entire process ranges greatly in duration, spanning from 6 months to 2 years. This duration will depend on the individual, severity, and rehabilitation.

Treatment for Frozen Shoulder
There are multiple treatment options for frozen shoulder ranging from both invasive and non-invasive options.
- Non-invasive
o Non-steroidal anti-inflammatory medicines: ask your family doctor about over the counter medications to help reduce your pain and inflammation.
o Physical therapy: physical therapy is a very common treatment option for frozen shoulder. There are many different approaches to helping rehabilitate from frozen shoulder including:
Education: your physiotherapist will start by explaining to you what frozen shoulder is, how it likely started, how to treat it and how long it will take. They will also be able to provide you with some strategies to help manage your pain (i.e. sleeping positions, positions to avoid etc.).
Pain Management: your physiotherapist may use various techniques to help you deal with pain. This can include modalities such as ultrasound or acupuncture, passive mobilizations, and stretching of surrounding musculature.
Increasing and maintaining shoulder mobility: your physiotherapist will work hands on with your affected shoulder to passively stretch the surrounding musculature as well as the shoulder joint capsule. This will be beneficial for maintaining your range of motion, as well as increasing it so there are no lasting limitations.
Home exercise program: your physiotherapist will provide you with an
individualized exercise program to manage your pain as well as progress
your shoulder range of motion. As your rehabilitation progresses, they will
progress your exercises as needed to ensure you are improving
appropriately.
- Invasive
o Intra-articular steroid injections: this is typically performed by a medical doctor, in which they will inject a corticosteroid into the shoulder capsule. The goal of the injection is to reduce swelling and inflammation.
o Manipulation under anesthesia: this is also typically performed by a medical doctor. During this procedure, you are given anesthetic and put to sleep. While under anesthesia, the doctor will move your shoulder with attempt to break up any adhesions or scar tissue.
o Shoulder arthroscopy: this is also performed by a medical doctor. During this procedure the doctor will make small incisions around your shoulder and using small instruments will cut tight portions in your joint capsule with the goal of freeing up range of motion.
If you have been diagnosed with frozen shoulder or think you may be suffering from frozen shoulder, call our clinic today to be assessed by one of our physiotherapists. They will help you with the management of your shoulder and help accelerate your rehabilitation so you can return to the activities you enjoy!
https://www.physionetwork.com/blog/frozen-shoulder-let-it-go-let-it-go/
https://orthoinfo.aaos.org/en/diseases–conditions/frozen-shoulder
https://www.physiotutors.com/frozen-shoulder-treatment/